Emergency Endotracheal Intubation: Ensuring Airway Patency in Critical Situations
ETT Size Guide:
- Adults:
- Most commonly used sizes in adults are between 7 & 8mm
- Sizes may vary according to the anatomical variations or abnormailities.
- Paediatrics:
- There is a formula to calculate the size of ETT in paediatric patients.
- ETT Size = [Age / 4 ] + 4
Endotracheal Intubation: Video
ETT Video
ETT Tips & Tricks
Emergency endotracheal intubation is a life-saving procedure used in critical situations to secure the airway and enable effective ventilation in patients who are unable to breathe adequately on their own. This article provides a concise overview of the key aspects of emergency endotracheal intubation, including indications, equipment required, procedure steps, and potential complications.
- Indications:
- Respiratory failure or impending respiratory failure.
- Inability to maintain a clear and patent airway.
- Trauma or injury affecting the airway.
- Cardiac arrest requiring advanced life support measures.
- Severe acute respiratory distress syndrome (ARDS).
- Management of upper airway obstruction or foreign body aspiration.
- Equipment Required:
- Endotracheal tube (ETT): A flexible tube inserted through the vocal cords into the trachea to secure the airway and allow for mechanical ventilation.
- Laryngoscope: A device with a handle and blade used to visualize the vocal cords and guide the placement of the endotracheal tube.
- Syringe: Used to inflate the cuff of the endotracheal tube once it is in the trachea.
- Stylet: A rigid wire that can be inserted into the endotracheal tube to provide shape and stiffness for easier insertion.
- Bag-mask ventilation device: Used for manual ventilation if needed before or after intubation.
- Monitoring equipment: Such as a pulse oximeter and capnography monitor, to assess the patient's oxygenation and ventilation status during the procedure.
- Procedure Steps:
- Preoxygenation:Administering high-flow oxygen to the patient to optimize oxygen reserves before the procedure.
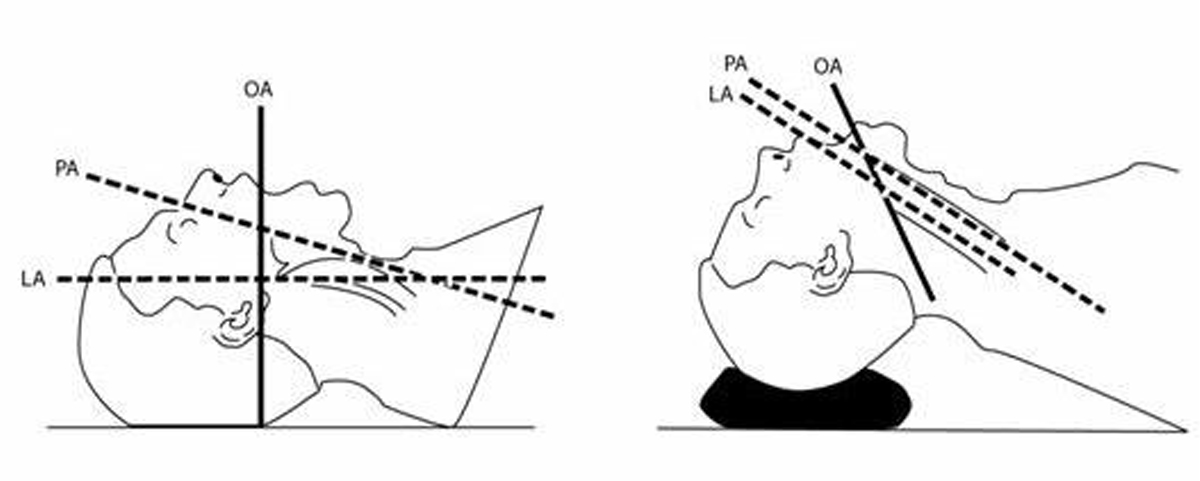
- Position the patient on the operating table with proper alignment along the Pharyngeal Axis.
- Rapid sequence induction (RSI):Administering an induction agent and a neuromuscular blocking agent to achieve unconsciousness and muscle relaxation.
- Laryngoscope Insertion and Visualization:
- Insert the blade:
- Hold the laryngoscope in the left hand (or non-dominant hand)
- Insert the blade of the laryngoscope into the right side of the fully open mouth
- Pass the blade to the right of the tongue
- Avoid contact with the soft tissues and teeth.
- Advance the blade:
- Advance the blade down the right side of the tongue
- “Sweep” the tongue to the left and out of the way
- Continue to advance the blade towards the base of the tongue
- Return the tip of the blade to the midline, identifying the epiglottis, prior to placing the tip into the vallecula.
- Lift the epiglottis:
- Use a moderate lifting force applied along the line of the laryngoscope handle (at a 45-degree angle to the floor) to lift the epiglottis and reveal the glottis
- Do not lever backwards on to the top teeth
- while doing this it is essential to maintain mouth opening and head and neck position.
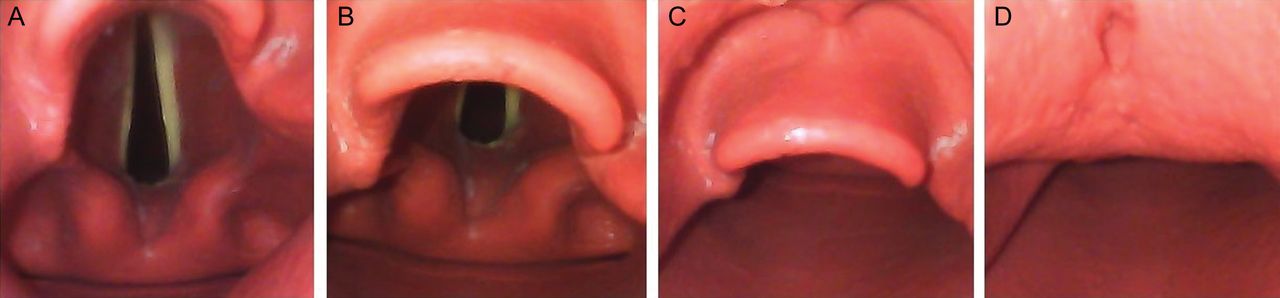
- Reveal the vocal cords:
- The larynx should now be visible
- Achieve the best view:
- Once the best view has been achieved, the anaesthetist should not take their eye off the vocal cords.
- Endotracheal Tube Insertion:
- Identify the appropriate time to perform the intubation based on the patient's clinical condition and assessment. Insert tube only if cords are visulized or ask for senior help.
- Maintain a view of the vocal cords while your assistant hands you the ETT
- Hold the ETT towards the proximal end
- Pass the ETT from the right side of the mouth, so that it can be seen approaching and entering the glottis in a direct line of sight (see image below)
- Advance the ETT until the cuff is about 2 cm distal to the vocal cords (many ETTs have a black mark, indicating the depth at the cords)
- Once positioned, take great care that the tube does not move. This is best done by holding the tube with your hand anchored on the patient’s cheek until the tube is secured.
- Inflating the Cuff and Confirmation:
- Your assistant will inflate the cuff to obtain a seal and prevent air leak from the lungs.
- your assistant will check the cuff pressure is within the normal range using a manometer.
- Confirmation:
- Visualise tube position through cords.
- Bilateral chest movement when squeezing the bag (visual +/– auscultation)
- You should see misting of the ETT
- ETCO2 capnography trace must be present – THIS IS CRUCIAL
- Once confirmed, secure the ETT with cotton bandage or paper-tape, whatever is avaialble.
- Securing the tube:Inflating the cuff of the endotracheal tube and securing it in place using tape or tube-holding devices.
- Complications:
- Difficult intubation or inability to visualize the vocal cords.
- Esophageal intubation or misplacement of the endotracheal tube.
- Hypoxia or desaturation during the procedure.
- Hemodynamic instability or changes in blood pressure and heart rate.
- Trauma to the airway structures or teeth.
- Aspiration of gastric contents.
- Infection or pneumonia.



Emergency endotracheal intubation is a vital intervention in critical situations to secure the airway and enable effective ventilation in patients who are unable to breathe adequately on their own. Proper training, expertise, and adherence to guidelines are crucial to ensure successful outcomes and minimize complications. The prompt and accurate execution of emergency endotracheal intubation can significantly improve patient outcomes and increase the chances of survival in life-threatening emergencies.
a project of alostmedic.com